NURS-6630C/6630N WK4Assgnent Newman
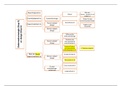
NURS-6630C/6630N WK4AssgnNewman NURS-6630C/6630N WK4AssgnNewman Decision Tree Week 4 An Asian American Woman with Bipolar Disorder Name NURS-6630C Psychopharmacologic Approaches to Treatment of Psychopathology Walden University Date An Asian American Woman with Bipolar Disorder Bipolar disorder (BD), also known as manic-depressive illness, is a brain disorder that causes unusual shifts in mood, energy, activity levels, and the inability to perform daily tasks. There are four fundamental types of bipolar disorder; all of which involve changes in mood, energy, and activity levels (Alda, 2015). Symptoms can result in unexpected mood and behavioral changes, giving rise to difficulties in life and resulting in significant distress (Alda, 2015). For Bipolar I disorder, the client has experienced at least one manic episode has taken place, which can be preceded or accompanied by hypomanic or major depressive episodes, mania, can in some instances cause psychosis (Grande, Berk, Birmaher & Vieta 2016). For Bipolar II, the client has experienced one significant episode of major depression and at least one episode of hypomania but never had a manic episode (Grande et al., 2016). Bipolar II disorder is a distinct diagnosis rather than a milder form of Bipolar I disorder. While the manic episodes of bipolar I disorder may be severe and harmful, clients with bipolar II disorder can suffer from depression for longer phases that may result in debilitating severe life challenges. In Cyclothymic disorder, the client has had many cycles of hypomania and episodes of depressive symptoms, though not as severe as major depression, continuing for at least two years in adults and one year in children and adolescents (Grande et al., 2016). Lastly, bipolar and related disorders induced by certain drugs or alcohol or due to a medical condition, such as Cushing's disease, multiple sclerosis or stroke can cause periods of significant depression and manic encounters (Grande et al., 2016). Bipolar disorder is a complicated condition, like all psychological disorders, with many variables, including a genetic predisposition for the disorder; therefore, a thorough, extensive examination of the client's clinical history must be conducted by the PMHNP according to Grande et al. (2016). The objective of this assignment is to give a contextual analysis of the Asian American woman with Bipolar disorder, taking into account pharmacokinetic and pharmacodynamic factors as well as any possible ethical considerations before offering treatment regimens. Client X Client X is a 26-year-old Asian American woman of Korean descent presenting today two weeks after discharge from a 21-day in-patient hospitalization for acute mania. Her diagnosis is Bipolar I disorder. This PMHNP has reviewed the hospital records, lab work shows WNL, unremarkable for any further medical conditions, and genetic testing (GeneSight) reveals she is positive for CYP2D6*10 allele (Chen et al., 2015). This testing was conducted as none of the medications during her 21-day hospitalization were effective. Upon arrival, Client X is increasingly engrossed in moving things on this PMHNP’s desk and fidgeting in her chair. During the initial exam client X reports she likes to talk, dance, sing and cook so she does not believe she can be Bipolar like the hospital told her she was. Client X spends much time looking for approval from this PMHNP. Client X says her mood is fantastic; she reports sleeping 5 hours a night but that she hates sleeping because it is not fun. Client X informs this PMHNP that the lithium the hospital prescribed for her she has not taken since she left the hospital two weeks ago. Her height 5’ 5” and weight 110 lbs., recorded by the nursing staff. The mental status exam was performed and client is alert and oriented x4. The client X is dressed in an evening gown for today's appointment, and her speech is rapid, pressured and tangential. She earlier reports her mood as fantastic and has a very intense affect. Client X denies any visual and auditory hallucinations as well as paranoid or delusional thoughts. This PMHNP notes judgment is impaired. Currently, client X denies suicidal or homicidal ideation or plans. The Young Mania Rating Scale (YMRS) was performed, and client X scored a 22. The Young Mania Rating Scale (YMRS) is a rating scale used to evaluate manic symptoms at baseline and over time in individuals with mania (Young, Biggs, Ziegler & Meyer [1978], 2019). Decision 1 For more than sixty years, lithium has been one of the most commonly researched and suggested medications for treating Bipolar disorder. According to Won and Kim (2017), lithium reduces the frequency and intensity of mania and if taken accordingly has the staying power to alleviate relapses. 60-70% of those diagnosed with Bipolar disorder report manic symptoms to decline while taking lithium (Findling et al., 2015). Some of the adverse side effects in taking lithium include diarrhea, vomiting, tremors, lack of coordination, drowsiness, and muscle weakness (Gitlin, 2016). Lithium is considered the first mood stabilizer to be approved by the US Food and Drug Administration (FDA) for the treatment of mania, however, due to the need for mania, depression and maintenance therapies, other drugs have recently been approved; Thorazine, Depakote, Zyprexa and Lamictal (Li et al., 2015). Decision point one challenges this PMHNP to prescribe Lithium 300mg orally BID, Risperdal 1mg orally BID, or Seroquel XR 100mg orally at HS. The immediate thought is to prescribed Lithium 300mg orally BID knowing from the recent hospitalization, and GeneSight testing proved the only medication to allow for discharge. Signs and symptoms demonstrated by client X show that she may be experiencing a manic episode brought on by her recent diagnosis of Bipolar I disorder. Background information provided as well as the results from the Young Mania Rating Scale (YMRS) proves evident she could be experiencing an episode. The choice for Lithium is, according to Won and Kim (2017), useful in those clients who present with fast cycling Bipolar disorder and can help to monitor current episodes of mania, which can be beneficial for client X at this given time. In examining the pharmacodynamics and pharmacokinetic properties of lithium, client X’s genetic testing for CYP2D6* 10 alleles will have some impact on the ingestion and bioavailability of lithium according to Ayano, (2016), as well as CYP2D6*10 allele is extremely common in populations of Asian ancestry (Chen et al., 2015). The effects of lithium can be separated by two groups; acute, which shows a decrease of manic symptoms within 5 to 7 days after the start of therapy, whereas, maintenance effects can be seen about the 21-day mark when system regulation has begun (Ayano, 2016). Starting where client X left off at discharge should be most effortless for client X to comprehend at this time. Risperdal known as atypical antipsychotic or a second-generation psychotic medication, would not be in client X’s best interest considering the adverse side effects such as weight increases, tardive dyskinesia and the risk of toxic concentrations from client X’s favorable CYP2D6*10 allele (Dean, 2017). Seroquel although an exceptional choice, works best in conjunction with another mood stabilizer, in particular by those who are considered fast-cycling when Bipolar disorder is diagnosed, like that of client X (Thase, 2018). The goal for client X is to reduce the manic episodes, avoid reoccurrence, and balance and maintain the medication regimen at a level client X can achieve, striving for a 25% reduction by the next visit. Also, for client X to develop a healthy sleeping pattern. Unfortunately, client X returns for her four weeks check-up with this PMHNP, she admits to only taking the Lithium 300mg orally BID when she feels she needs it. Client X’s behavior was unchanged from the first encounter four weeks ago. With client X’s medication regime non-compliance as well as her lack of ability to comprehend that compliance is necessary to attain favorable results, it is evident that this PMHNP did not communicate the intended outcomes and the decision was not favorable. Decision 2 Modifications must be done in order for client X to be successful. After prescribing Lithium 300mg orally BID, the next steps must be approached with an educational rationale for client X’s success. The choices for modifying client X’s care plan consist of increasing Lithium to 450mg orally BID, assess rational for non-compliance to elicit reason for non-compliance and educate client of the drug effects and pharmacology, or switch entirely to Depakote ER 500mg orally at HS. The previous history of client X’s failure to comply during her 21-day hospitalization as well as the past four-week trial on Lithium 300mg orally BID, this PMHNP is reluctant but compelled to change the medication regimen to Depakote ER 500mg orally at HS. Perhaps this will encourage client X the importance of adherence and to allow for success instead of inconsistency by the one time a day change occurring at bedtime. The antiepileptic agent Depakote is an alternative for patients with mania who cannot tolerate lithium or for whom it was ineffective for multiple reasons (Stoner & Dahmen 2017). Depakote ER’s formulation should be considered a safe alternative, mainly when there is a history for concern of adverse events or when once-daily dosing is preferred to enhance compliance (Stoner & Dahmen 2017). However, long-term side effects that have been associated with Depakote are weight gain and liver damage (Nierenberg, 2010); therefore, educating client X about these possible adverse effects will be crucial in her compliance. The decision by this PMHNP to forego increasing the dose of Lithium to 450mg orally BID was simply due to client X’s initial non-compliance. Increasing the dose would not increase the chance of client X’s adherence to the treatment plan. However, educating client X does play a part in decision point #2 as according to Ratheesh et al. (2017), medication dosing has been deemed a significant role in those with Bipolar disorder and their reasoning behind non-compliance therefore, assessment and education should be conducted in conjunction with the newly prescribed Depakote 500mg ER orally at HS. First and foremost, the goal for client X is compliance. Without compliance, manic symptoms will have no significant changes. Patients should be monitored closely for the appearance of these symptoms. Serum liver tests should be performed before therapy and at frequent intervals after that, especially during the first six months as well as a pregnancy test to rule out the possibility of Depakote harming an unborn fetus (Stoner & Dahmen 2017). This PMHNP should educate client X on the possible side effects as well as the significance of adhering to the medication treatment plan in order to improve her present conditions. Upon client X’s return after four weeks on Depakote 500mg ER orally at HS, this PMHNP notices a decrease in manic symptoms in the initial visit. The Young Mania Rating Scale (YMRS) was conducted by this PMHNP, and client X scored an 11, which is down 50% (22) from 8 weeks ago. In the conversation with client X, she reports she had gained 6 pounds since our last visit four weeks ago, and she wants to stop taking the medication. Client X’s weight was taken, and her weight is 116 pounds to date, indicating an increase to match her reported gain. According to this PMHNP it appears that client X has been compliant with medication in the past four weeks and manic symptoms have decreased. Decision 3 Presumably, this PMHNP has discussed with client X the adverse effects of Depakote 500mg ER at HS; weight gain is the focus at this point. The choices to present client X at this point would be to continue the Depakote 500mg ER orally at HS and further the education and turn the attention to diet, exercise, and weight loss so that client X can remain successful in lowering the manic episodes, or to decrease the dosing of Depakote to 250mg ER orally at HS, or switch medications and start Zyprexa 15mg orally at HS. The decision to hold steady at the current dosing of Depakote 500mg daily orally at HS while educating client X on healthy diet and exercise, striving for continued reduction of manic symptoms and success in medication compliance will be this PMHNP’s choice. The reduction of Depakote dosing would not benefit client X in way that she would see or feel enough benefit. Client X has had a reduction in manic symptoms shown in the results of the Young Mania Rating Scale (YMRS), therefore lowering the dosage will then reverse the outcome of the treatment plan as well as her weight would not fluctuate enough and might cause client X to abandon treatment altogether. The decision to change medications to Zyprexa 15mg orally daily at HS will not change the time in which client X is scheduled to take the medication, so therefore, she could show success in remaining vigilant with adhering to her treatment plan. However, Zyprexa, according to Goldberg and Ernst (2018) state the adverse effects on those with Bipolar disorder is significant weight gain. The results show that Zyprexa monotherapy is associated with significantly more weight gain than other bipolar disorder medications such as lithium, Depakote, haloperidol, and risperidone and that are known to cause moderate weight gain (Nashed, Restivo, & Taylor, 2011). Ethical Considerations Client X is an Asian American woman of Korean descent of which this PMHNP needs to be socially and culturally aware of how mental health is perceived not only by client X but also by those who support her, making sure that the goal of treatment remains morally respectful. Providing client X with appropriate consequences and benefits of medication compliance and other treatment offerings will be beneficial to successful therapy outcomes (Ratheesh et al., 2017). The objective is to find common ground with a trusted working relationship while encouraging client X to assume responsibility, engage in the treatment plan and its expected outcome (Ratheesh et al., 2017). Conclusion There is no single cause for bipolar disorder; however, the complexity of Bipolar disorder along with multiple contributing factors such as genetics account for 60% - 80% of genetic factors of Bipolar disorder in families (Miziou et al., 2015). Bipolar disorder is an extremely persistent disease which is depicted by the inability to carry out activities of daily living to the extreme, suicidal ideation (Grande et al., 2016). Despite being a lifelong condition, often diagnosed in teenage years, mood swings and other generalized symptoms of Bipolar disorder can be managed with a medication treatment regimen, therapy plan, a dedicated PMHNP, and the willingness of the client (MacQueen & Memedovich, 2017). The primary focus in the treatment of bipolar disorder is mood stabilization (Nierenberg, 2010), of which only a few medications demonstrate positive results. Bipolar disorder related challenges include adverse reactions to medications, lack of prolonged periods or times of excitement, lack of family and community support, and lack of compliance (MacQueen & Memedovich, 2017). For more than sixty years, for those diagnosed with Bipolar disorder, lithium has been one of the most highly recommended medications with the ability to reduce the manic episodes, in those clients reporting adherence to medication regimens (Alda, 2015). Non-compliance is a critical issue for long term treatment of Bipolar disorder with repetitive indications (Alda, 2015). In conclusion, when prescribing lithium or any medication for Bipolar disorder, it is imperative that PMHNP’s incorporate education into treatment plans and highlight the adverse effects as well as the benefits for positive outcomes (Nierenberg, 2010). References Alda, M. (2015). Lithium in the treatment of bipolar disorder: pharmacology and pharmacogenetics. Molecular psychiatry, 20(6), 661. Ayano, G. (2016). Bipolar disorders. Pharmacokinetics, pharmacodynamics and therapeutic effects and indications: review of articles. Bipolar Disorder, 2(109), . Chen, R., Wang, H., Shi, J., Shen, K., & Hu, P. (2015). Cytochrome P450 2D6 genotype affects the pharmacokinetics of controlled-release paroxetine in healthy Chinese subjects: comparison of traditional phenotype and activity score systems. European Journal of Clinical Pharmacology, 71(7), 835-841. doi:10.1007/s Dean L. (2017). Risperidone Therapy and CYP2D6 Genotype. 2017 Apr 10. In: Pratt V, McLeod H, Rubinstein W, et al., editors. Medical Genetics Summaries [Internet]. Bethesda (MD): National Center for Biotechnology Information (US); 2017-. Available from: Findling, R. L., Robb, A., McNamara, N. K., Pavuluri, M. N., Kafantaris, V., Scheffer, R., & Rowles, B. M. (2015). Lithium in the acute treatment of bipolar I disorder: a double- blind, placebo-controlled study. Pediatrics, 136(5), 885-894. Gitlin, M. (2016). Lithium side effects and toxicity: prevalence and management strategies. International journal of bipolar disorders, 4(1), 27. Goldberg, J. F., & Ernst, C. L. (2018). Managing the side effects of psychotropic medications. American Psychiatric Pub. Grande, I., Berk, M., Birmaher, B., & Vieta, E. (2016). Bipolar disorder. The Lancet, 387(10027), . Li, X. B., Tang, Y. L., Wang, C. Y., & de Leon, J. (2015). Clozapine for treatment‐resistant bipolar disorder: a systematic review. Bipolar disorders, 17(3), 235-247. MacQueen, G. M., & Memedovich, K. A. (2017). Cognitive dysfunction in major depression and bipolar disorder: Assessment and treatment options. Psychiatry and clinical neurosciences, 71(1), 18-27. Miziou, S., Tsitsipa, E., Moysidou, S., Karavelas, V., Dimelis, D., Polyzoidou, V., & Fountoulakis, K. N. (2015). Psychosocial treatment and interventions for bipolar disorder: a systematic review. Annals of general psychiatry, 14(1), 19. Nashed, M. G., Restivo, M. R., & Taylor, V. H. (2011). Olanzapine-induced weight gain in patients with bipolar I disorder: a meta-analysis. The primary care companion for CNS disorders, 13(6), PCC.11r01174. doi:10.4088/PCC.11r01174 Nierenberg A. A. (2010). A critical appraisal of treatments for bipolar disorder. Primary care companion to the Journal of clinical psychiatry, 12(Suppl 1), 23–29. doi: 10.4088/PCC.9064su1c.04 Ratheesh, A., Cotton, S. M., Davey, C. G., Adams, S., Bechdolf, A., Macneil, C., & McGorry, P. D. (2017). Ethical considerations in preventive interventions for bipolar disorder. Early intervention in psychiatry, 11(2), 104-112. Stoner, S. C., & Dahmen, M. M. (2017). Extended-release divalproex in bipolar and other psychiatric disorders: A comprehensive review. Neuropsychiatric disease and treatment, 3(6), 839–846. doi:10.2147/ndt.s1264 Thase, M. E. (2018). Quetiapine monotherapy for bipolar depression. Neuropsychiatric disease and treatment, 4(1), 11–21. Won, E., & Kim, Y. K. (2017). An oldie but goodie: lithium in the treatment of bipolar disorder through neuroprotective and neurotrophic mechanisms. International journal of molecular sciences, 18(12), 2679. Young, R., Biggs, J., Ziegler, V., Meyer, D. (2019). A rating scale for mania: reliability, validity and sensitivity. Br J Psychiatry. 1978; 133:429-435.
Geschreven voor
Documentinformatie
- Geüpload op
- 28 augustus 2021
- Aantal pagina's
- 12
- Geschreven in
- 2021/2022
- Type
- Case uitwerking
- Docent(en)
- Professor
- Cijfer
- A
Onderwerpen
-
nurs 6630c6630n wk4assgnnewman decision tree week 4 an asian american woman with bipolar disorder name nurs 6630c psychopharmacologic approaches to treatment of psychopathology walden uni