Arterial Blood Gas For Dummies!
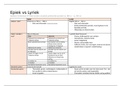
Respiratory Side Metabolic Side
CO2 VS HCO3 (Bicarb)
Lungs VS Kidneys
Can be changed instantly VS Takes at least 24 hours to change
(Tidal volume, Inc RR)
pH: 7.35-7.45
PO2: 80-100mm Hg* 60-79 mild, 40-59 moderate, <40 is severe hypoxemia
PaCO2: 35-45 (ACID)
BiCarb (HC03): 22-26 (BASE)
Base Excess: -2 to +2 * Most reliable index of metabolic acidosis
*PO2 Normal changes with age – subtract 1 for each year over 60 from 80 for low value on room air.
O2 sat- 30-60-90 rule: P02 of 30 is O2 sat of 60%, 60 is 90%, 90 is 95% saturated.
-- Hypoxia is #1 reason for met. acidosis so INCREASE OXYGEN!!!
Signs of Acidosis:
• CNS depression, Headache, lethargy, weakness, confusion, coma, kussmaul respirations
Signs of Alkalosis:
• CNS Irritability, restlessness, twitches, tingles, numb fingers, tetany, seizure, coma
Assessment of Acid Base Imbalance
• If the pH is off, check the PCO2. If both are acidotic, then the cause is respiratory. If pH is low and PCO2 is also
low, then it must be metabolic with respiratory compensation.
• If base excess follows the pH, it’s metabolic. If it’s opposite, then it’s metabolic compensation.
Page 1 of 28
, Care of Ventilated Patients
Artificial Airways
- Short term
1. Oropharyngeal Airway
* Very sedated, Altered LOC, Patient must have no gag reflex, no aspiration
* KEEPS AIRWAY OPEN ONLY!
2. Nasopharyngeal Airway
* Lubricate liberally with insertion! Can have gag reflex and use.
3. Endotracheal tubes (intubation)
- Long Term
4. Tracheostomy tubes
3. Endotracheal Tubes
- Most common for SHORT TERM airway management.
- no air should be coming out of anywhere except tube!
- Patient should NOT be able to speak. If so, it is probably dislodged
- Indications
• Maintain airway patency
• Protect from aspiration (Balloon)
• Positive-pressure ventilation (creates a seal)
• Facilitate pulmonary toileting (Suctioning)
• Provide high oxygen concentrations if needed
- Naso vs. Orotracheal== Naso has increased infection risk. Orotracheal most likely unless oral trauma!
o Nasal is preferred for elective insertion when the patient is capable of spontaneous ventilation for a short
period. Nasal is more comfortable. Typically used for conscious patients who are at risk for imminent resp
arrest or who cervical spinal injuries.
o DO NOT use Nasal for pts with facial or basilar skull fractures. This way causes more tissue damage and
increases risk of infection by nasal bacteria introduced into the trachea and increases the risk of pressure
necrosis of the nasal mucosa.
- Balloon can cause necrosis if left inflated in the throat to long—NOT OVER 2 WEEKS!
- Blue port outside of mouth also has balloon to check for patency of unseen balloon
- Size 6-7 for women; Size 7-8 for men.
- Assistance with intubation
* Equipment
- Suction setup (canister, tubing, vacuum head)
~ suck secretions before intubating so you’re not pushing them farther into lungs!
~ Check balloon patency before inserting!!
- Yaunker
- OETT
- Lubricant!!!!
- Stylet
~ a long piece of metal to help firm tube in order to help insertion. Stylet cannot pass the end
of tube or can cause perforation of lung
- Laryngoscope
- Valve-bag mask with 100% FiO2
- Continuous SaO2 monitor
Page 2 of 28
, - Medications
~ Sedative/paralytic necessary if intubating patient who is awake!
>Wait til doctor is READY to do procedure. Paralytic will cause pt to stop breathing
completely!
> Sedative first then paralytic (Make sure you’re allowed to push sedative!—Scope of
practice—may need an anesthesiologist)
Endotracheal Tubes Cont.
- Confirmation of placement
* Chart how deep it is—Ex. 25 at lip
* Tip of tube should be 3 to 4 cm. above carina (where stems branch off to separate lungs)
1. Bilateral breath sounds (ER)
- None in abdomen, absence of gurgling!!
- If only one lung, then tube was put in to far!
2. CO2 detector (ER)
- goes on end of tube
- If turns yellow on exhale then correct placement!
3. CXR (BEST!!! But takes longest)
-- Not definitive BUT if you put deflated bulb syringe into end of tube and it pops open then correct placement!
Tracheostomy Tubes (Long term) Dec. infection risk!
Advantages:
1. Avoids oral, nasal, pharyngeal, and laryngeal complications/trauma/necrosis
2. Shorter with a wide diameter (SOO decreased air resistance & easier to wean)
- Compare breathing through a straw to breathing through a water hose
3. Less curved with easier secretion removal
4. Increased comfort
5. Able to eat and talk!!!!!
- Components:
* Made of plastic (MOST!) or metal
* Tube
* Cuff
* Obturator
- helps with insertion
- little piece of plastic
- holds place in case tube falls out so KEEP ONE AT BEDSIDE!!!
* Inner Cannula
- Either removable or replaceable so easier to clean!
- Indications:
* Extrapulmonary
- CNS, Neuromuscular
- Muscular
~ Action: interrupted of inhibited movement of chest wall
> Flail chest (broken ribs—unable to pull air in)
Page 3 of 28
Respiratory Side Metabolic Side
CO2 VS HCO3 (Bicarb)
Lungs VS Kidneys
Can be changed instantly VS Takes at least 24 hours to change
(Tidal volume, Inc RR)
pH: 7.35-7.45
PO2: 80-100mm Hg* 60-79 mild, 40-59 moderate, <40 is severe hypoxemia
PaCO2: 35-45 (ACID)
BiCarb (HC03): 22-26 (BASE)
Base Excess: -2 to +2 * Most reliable index of metabolic acidosis
*PO2 Normal changes with age – subtract 1 for each year over 60 from 80 for low value on room air.
O2 sat- 30-60-90 rule: P02 of 30 is O2 sat of 60%, 60 is 90%, 90 is 95% saturated.
-- Hypoxia is #1 reason for met. acidosis so INCREASE OXYGEN!!!
Signs of Acidosis:
• CNS depression, Headache, lethargy, weakness, confusion, coma, kussmaul respirations
Signs of Alkalosis:
• CNS Irritability, restlessness, twitches, tingles, numb fingers, tetany, seizure, coma
Assessment of Acid Base Imbalance
• If the pH is off, check the PCO2. If both are acidotic, then the cause is respiratory. If pH is low and PCO2 is also
low, then it must be metabolic with respiratory compensation.
• If base excess follows the pH, it’s metabolic. If it’s opposite, then it’s metabolic compensation.
Page 1 of 28
, Care of Ventilated Patients
Artificial Airways
- Short term
1. Oropharyngeal Airway
* Very sedated, Altered LOC, Patient must have no gag reflex, no aspiration
* KEEPS AIRWAY OPEN ONLY!
2. Nasopharyngeal Airway
* Lubricate liberally with insertion! Can have gag reflex and use.
3. Endotracheal tubes (intubation)
- Long Term
4. Tracheostomy tubes
3. Endotracheal Tubes
- Most common for SHORT TERM airway management.
- no air should be coming out of anywhere except tube!
- Patient should NOT be able to speak. If so, it is probably dislodged
- Indications
• Maintain airway patency
• Protect from aspiration (Balloon)
• Positive-pressure ventilation (creates a seal)
• Facilitate pulmonary toileting (Suctioning)
• Provide high oxygen concentrations if needed
- Naso vs. Orotracheal== Naso has increased infection risk. Orotracheal most likely unless oral trauma!
o Nasal is preferred for elective insertion when the patient is capable of spontaneous ventilation for a short
period. Nasal is more comfortable. Typically used for conscious patients who are at risk for imminent resp
arrest or who cervical spinal injuries.
o DO NOT use Nasal for pts with facial or basilar skull fractures. This way causes more tissue damage and
increases risk of infection by nasal bacteria introduced into the trachea and increases the risk of pressure
necrosis of the nasal mucosa.
- Balloon can cause necrosis if left inflated in the throat to long—NOT OVER 2 WEEKS!
- Blue port outside of mouth also has balloon to check for patency of unseen balloon
- Size 6-7 for women; Size 7-8 for men.
- Assistance with intubation
* Equipment
- Suction setup (canister, tubing, vacuum head)
~ suck secretions before intubating so you’re not pushing them farther into lungs!
~ Check balloon patency before inserting!!
- Yaunker
- OETT
- Lubricant!!!!
- Stylet
~ a long piece of metal to help firm tube in order to help insertion. Stylet cannot pass the end
of tube or can cause perforation of lung
- Laryngoscope
- Valve-bag mask with 100% FiO2
- Continuous SaO2 monitor
Page 2 of 28
, - Medications
~ Sedative/paralytic necessary if intubating patient who is awake!
>Wait til doctor is READY to do procedure. Paralytic will cause pt to stop breathing
completely!
> Sedative first then paralytic (Make sure you’re allowed to push sedative!—Scope of
practice—may need an anesthesiologist)
Endotracheal Tubes Cont.
- Confirmation of placement
* Chart how deep it is—Ex. 25 at lip
* Tip of tube should be 3 to 4 cm. above carina (where stems branch off to separate lungs)
1. Bilateral breath sounds (ER)
- None in abdomen, absence of gurgling!!
- If only one lung, then tube was put in to far!
2. CO2 detector (ER)
- goes on end of tube
- If turns yellow on exhale then correct placement!
3. CXR (BEST!!! But takes longest)
-- Not definitive BUT if you put deflated bulb syringe into end of tube and it pops open then correct placement!
Tracheostomy Tubes (Long term) Dec. infection risk!
Advantages:
1. Avoids oral, nasal, pharyngeal, and laryngeal complications/trauma/necrosis
2. Shorter with a wide diameter (SOO decreased air resistance & easier to wean)
- Compare breathing through a straw to breathing through a water hose
3. Less curved with easier secretion removal
4. Increased comfort
5. Able to eat and talk!!!!!
- Components:
* Made of plastic (MOST!) or metal
* Tube
* Cuff
* Obturator
- helps with insertion
- little piece of plastic
- holds place in case tube falls out so KEEP ONE AT BEDSIDE!!!
* Inner Cannula
- Either removable or replaceable so easier to clean!
- Indications:
* Extrapulmonary
- CNS, Neuromuscular
- Muscular
~ Action: interrupted of inhibited movement of chest wall
> Flail chest (broken ribs—unable to pull air in)
Page 3 of 28