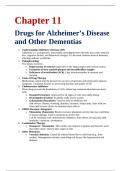
Drugs for Alzheimer’s Disease
and Other Dementias
1. Understanding Alzheimer’s Disease (AD)
Alzheimer’s is a progressive, irreversible neurodegenerative disorder that causes memory
loss, cognitive decline, and behavioral changes. It’s the most common form of dementia,
affecting millions worldwide.
2. Pathophysiology
The disease involves:
o Degeneration of neurons (especially in the hippocampus and cerebral cortex)
o Formation of beta-amyloid plaques and neurofibrillary tangles
o Deficiency of acetylcholine (ACh), a key neurotransmitter in memory and
learning
3. Goals of Drug Therapy
Medications cannot stop the disease but can slow progression and temporarily improve
symptoms. Treatment focuses on preserving function and quality of life.
4. Cholinesterase Inhibitors
These drugs prevent the breakdown of ACh, enhancing communication between nerve
cells:
o Donepezil (Aricept): Approved for all stages of AD; once-daily dosing
o Rivastigmine (Exelon): Available orally and as a patch
o Galantamine (Razadyne): Used for mild-to-moderate AD
Side effects: Nausea, vomiting, diarrhea, dizziness, bradycardia. Start with low
doses and increase slowly to minimize these effects.
5. NMDA Receptor Antagonist
o Memantine (Namenda): Blocks excessive glutamate activity that may contribute
to neuron damage. Used in moderate-to-severe AD.
Can be combined with cholinesterase inhibitors. Side effects are typically mild:
headache, confusion, constipation.
6. Combination Therapy
o Donepezil + Memantine: This combo may improve cognition and function more
than either alone. Used in later stages of AD.
7. Other Dementias
o Vascular dementia: Caused by reduced blood flow to the brain (e.g., from
strokes). Management includes controlling risk factors like hypertension and
diabetes.
, o Lewy body dementia: Characterized by hallucinations, movement issues, and
fluctuating alertness. Cholinesterase inhibitors may help. Antipsychotics must be
used cautiously.
o Frontotemporal dementia: Affects behavior and language. No FDA-approved
treatments; SSRIs may help with behavioral symptoms.
8. Behavioral Symptoms Management
o Agitation, aggression, delusions, and sleep disturbances are common.
o Non-drug approaches (e.g., routines, redirection) are first-line.
o Low-dose antipsychotics (e.g., risperidone) may be used with extreme caution
due to increased risk of death in elderly patients with dementia.
9. Patient and Caregiver Support
Education, support groups, and respite care help reduce caregiver stress and improve
patient outcomes. Regular monitoring is important to evaluate treatment benefits and
adjust care plans.
, Chapter 12
Drugs for Seizure Disorders
1. Understanding Seizure Disorders
Seizures are caused by sudden, abnormal electrical activity in the brain. They may result
from epilepsy, brain injury, tumors, infections, or metabolic imbalances. Seizures vary in
type and severity.
2. Types of Seizures
o Focal (partial) seizures: Originate in one area of the brain. May be simple (no
loss of awareness) or complex (impaired consciousness).
o Generalized seizures: Involve both brain hemispheres. Includes tonic-clonic,
absence, myoclonic, and atonic seizures.
3. Goals of Drug Therapy
The aim is to reduce or eliminate seizures while minimizing side effects. Treatment must
be individualized based on seizure type, frequency, and patient-specific factors.
4. Mechanism of Action for Antiepileptic Drugs (AEDs)
AEDs work by:
o Suppressing abnormal neuron firing
o Enhancing inhibitory neurotransmitters (e.g., GABA)
o Inhibiting excitatory neurotransmitters (e.g., glutamate)
o Blocking sodium or calcium channels
5. Common AEDs and Their Uses
o Phenytoin (Dilantin): Effective for focal and tonic-clonic seizures; narrow
therapeutic index
o Carbamazepine (Tegretol): Used for focal seizures, trigeminal neuralgia, bipolar
disorder
o Valproic acid (Depakote): Broad-spectrum; treats generalized seizures, bipolar
disorder, migraines
o Lamotrigine (Lamictal): Also for mood stabilization; risk of serious skin rash
o Levetiracetam (Keppra): Well-tolerated; used for focal and generalized seizures
o Topiramate (Topamax): Also for migraines and weight loss; risk of cognitive
side effects
6. Side Effects and Monitoring
o CNS effects: Drowsiness, dizziness, blurred vision
o GI effects: Nausea, vomiting
o Hematologic/liver toxicity: Monitor labs (e.g., liver function, CBC)
o Skin reactions: Rash (especially with lamotrigine or phenytoin)
7. Drug Interactions
Many AEDs induce or inhibit liver enzymes (especially CYP450), altering levels of other