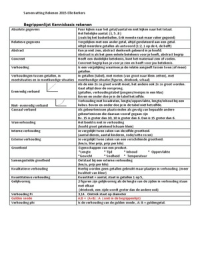
Hypertension (HTN) Angina
Definition clinic reading persistently above ≥ 140/90 mmHg OR 24hr BP average Definition substernal discomfort that I precipitated by exercise but relieve
reading ≥ 135/85 mmHg by rest/GTN spray
Pathophysiology Aetiology
1. Primary/essential (95%)- unknown Atherosclerosis – underlying cause of IHD when it occurs in coronary
2. Secondary
arteries
Renal glomerulonephritis, chronic pyelonephritis, APKD, renal artery
stenosis 1. Fatty streak formation lipid deposition in intima inflammation,
Endocrine primary hyperaldosteronism, phaeochromocytoma, Cushing’s, increased permeability, increased WBC Macrophages
CAH, Acromegaly, Liddle phagocytose lipids foam cells
Other glucocorticoids, NSAIDs, pregnancy, CoA, COCP 2. Fibrolipid plaque lipid in intima stimulates fibrocollagenous tissue
Cushing’s + Conn’s = High aldosterone + Low renin causes thinning of muscular media
RAS = High aldosterone + High renin
3. Complicated atheroma plaque is extensive, prone to rupture +
Liddle= Low aldosterone + Low renin
Signs + symptoms calcified
Usually asymptomatic unless very high i.e. > 200/120mmHg Rarely anaemia/tachyarrhythmia
Headaches
Visual disturbances Classification
Seizures Stable Discomfort on exertion, reduced w/ rest ST depression
Classification Unstable Discomfort by rest/minimal exertion ST depression
Clinical reading of ≥ 140/90 mmHg ABPM/HBPM:
Decubitus Triggered by lying flat ST depression
< 135/85 Not hypertensive
> 135/85 Stage1 Rx if < 80 y/o and either: Prinzmetal Due to coronary artery spasm ST elevation during
Target organ damage, Renal disease, Diabetes, CVD, CV 10 year the attack which resolves as pain subsides
risk > 20% Ix ‘ECG’
> 150/95 Stage 2 Rx all, regardless of age ECG signs of ST depression/ST elevation (Exercise ECG no longer
Ix Check for end- organ damage recommended)
1. Fundoscopy HTN retinopathy? CT scan, Coronary Calcium score (measured on CT)
2. Urine dipstick Renal disease?
Go for thallium scan (myocardial perfusion)
3. ECG LVH/Ischaemic HD?
Mx
< 55 years > 55 years/Afro-Caribbean Mx
1. Conservative
ACEi/ARB Calcium channel blocker 2. Medical
Step 1 e.g. Lisinopril/ Candesartan e.g. Nifedipine/Amlodipine
GTN (spray/SL) + aspirin + statin
Step 2 ACE + CCB β- blocker e.g. Atenolol / CCB e.g. Verapamil/Diltiazem
Step 3 ACE + CCB + Diuretic (Thiazide) e.g. Chlorthalidione/Indapamide monotherapy
Step 4 If K+ ≤ 4.5 Spironolactone Switch to alternative monotherapy
If K + ≥ 4.5 High-dose thiazide diuretic Combination therapy
If further diuretic therapy not tolerated consider α/β- blocker (Note: use Nifedipine/Amlodipine as CCB since β- blocker
New drugs Renin blockers e.g. Aliskiren + verapamil heart block)
Blocks angiotensinogen ATI Still no improvement
Trials have only looked at fall in BP, as effective as ACEi/ARB ISMN/slow-release nitrate, Ivabradine, Nicorandil,
SE: uncommon, other than diarrhoea
Ranolazine
Definition clinic reading persistently above ≥ 140/90 mmHg OR 24hr BP average Definition substernal discomfort that I precipitated by exercise but relieve
reading ≥ 135/85 mmHg by rest/GTN spray
Pathophysiology Aetiology
1. Primary/essential (95%)- unknown Atherosclerosis – underlying cause of IHD when it occurs in coronary
2. Secondary
arteries
Renal glomerulonephritis, chronic pyelonephritis, APKD, renal artery
stenosis 1. Fatty streak formation lipid deposition in intima inflammation,
Endocrine primary hyperaldosteronism, phaeochromocytoma, Cushing’s, increased permeability, increased WBC Macrophages
CAH, Acromegaly, Liddle phagocytose lipids foam cells
Other glucocorticoids, NSAIDs, pregnancy, CoA, COCP 2. Fibrolipid plaque lipid in intima stimulates fibrocollagenous tissue
Cushing’s + Conn’s = High aldosterone + Low renin causes thinning of muscular media
RAS = High aldosterone + High renin
3. Complicated atheroma plaque is extensive, prone to rupture +
Liddle= Low aldosterone + Low renin
Signs + symptoms calcified
Usually asymptomatic unless very high i.e. > 200/120mmHg Rarely anaemia/tachyarrhythmia
Headaches
Visual disturbances Classification
Seizures Stable Discomfort on exertion, reduced w/ rest ST depression
Classification Unstable Discomfort by rest/minimal exertion ST depression
Clinical reading of ≥ 140/90 mmHg ABPM/HBPM:
Decubitus Triggered by lying flat ST depression
< 135/85 Not hypertensive
> 135/85 Stage1 Rx if < 80 y/o and either: Prinzmetal Due to coronary artery spasm ST elevation during
Target organ damage, Renal disease, Diabetes, CVD, CV 10 year the attack which resolves as pain subsides
risk > 20% Ix ‘ECG’
> 150/95 Stage 2 Rx all, regardless of age ECG signs of ST depression/ST elevation (Exercise ECG no longer
Ix Check for end- organ damage recommended)
1. Fundoscopy HTN retinopathy? CT scan, Coronary Calcium score (measured on CT)
2. Urine dipstick Renal disease?
Go for thallium scan (myocardial perfusion)
3. ECG LVH/Ischaemic HD?
Mx
< 55 years > 55 years/Afro-Caribbean Mx
1. Conservative
ACEi/ARB Calcium channel blocker 2. Medical
Step 1 e.g. Lisinopril/ Candesartan e.g. Nifedipine/Amlodipine
GTN (spray/SL) + aspirin + statin
Step 2 ACE + CCB β- blocker e.g. Atenolol / CCB e.g. Verapamil/Diltiazem
Step 3 ACE + CCB + Diuretic (Thiazide) e.g. Chlorthalidione/Indapamide monotherapy
Step 4 If K+ ≤ 4.5 Spironolactone Switch to alternative monotherapy
If K + ≥ 4.5 High-dose thiazide diuretic Combination therapy
If further diuretic therapy not tolerated consider α/β- blocker (Note: use Nifedipine/Amlodipine as CCB since β- blocker
New drugs Renin blockers e.g. Aliskiren + verapamil heart block)
Blocks angiotensinogen ATI Still no improvement
Trials have only looked at fall in BP, as effective as ACEi/ARB ISMN/slow-release nitrate, Ivabradine, Nicorandil,
SE: uncommon, other than diarrhoea
Ranolazine