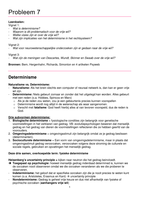
Anaphylaxis Status epilepticus Neonatal Resuscitation Diabet
Compli
Most c
C: 6 hours 12 hours infectio
Anaphylactic reaction? Assess Birth
Review biochemical + metabolic parameters (check Clinica
Airway Breathing Circulation venous pH, HCO3, K+, BM, ketones) Abdom
breath
Dx Cri
Assess Dry the baby Glucos
Airway Breathing Circulation Disability Maintain
D: 12 24normal
hourstemperature pH <7.
Exposure Check blood glucose By 24 hours- ketonaemia + acidosis should have HCO3 <
If blood glucose <3 mmol/L, give glucose IV and Ketone
resolved
recheck blood glucose Ix
Assess (tone), breathing, HR BM + k
E: Conversion to subcutaneous insulin metabo
Diagnosis (T wav
Acute onset of illness Vascular access No vascular
Airway swelling, hoarseness, stridor Lorazepram 0.1 mg/kg access If gasping/not breathing
Breathing tachypnoea, wheeze, cyanosis, Diazepam 0.5mg/kg Give 5 inhalation breaths
SpO2 <92% PR Consider SpO2 +/- ECG
OR midazolam
Circulation pale, clammy, hypotension, No response in 10
drowsy, coma mins
(buccal) 0.5 mg/kg
DK
Skin changes Re-assess
+/- GI symptoms If no increase in HR look for chest
Lorazepram 0.1mg/kg IV movement during inflation
No response in 10 mins
If chest not moving When the chest A:
Re-check head is moving
Call for help position
Res
Paraldehyde 0.4 ml/kg PR Consider 2-person
If the HR is not ove
airway control + detectable/is Mo
other airway very slow Pot
Lie patient flat and raise legs (if breathing manoeuvres (<60/min) Com
not impaired) No response in 10 mins Repeat inflation
Call for senior help ventilate for 30
breaths
SpO2 +/- ECG
seconds
Look for a response
Adrenaline (1:1000)
Phenytoin
Phenobarbital Reassess HR
Sodium valproate If still <60/min start chest
compressions; coordinate with
If available Monitor ventilation breaths (ratio 3:1)
Establish airway Pulse oximetry
High flow O2 ECG
Blood pressure Call anaesthetist/ no response in 20
IV fluid (20ml/kg mins
crystalloids) Re-assess HR every 30 seconds
Chlorpheniramine (IM/slow Rapid-sequence induction with thiopental If HR is not detectable/ very slow
IV) Mechanical ventilation (<60/min) consider venous
Hydrocortisone (IM/ slow Transfer to PICU access/drugs
IV)
Compli
Most c
C: 6 hours 12 hours infectio
Anaphylactic reaction? Assess Birth
Review biochemical + metabolic parameters (check Clinica
Airway Breathing Circulation venous pH, HCO3, K+, BM, ketones) Abdom
breath
Dx Cri
Assess Dry the baby Glucos
Airway Breathing Circulation Disability Maintain
D: 12 24normal
hourstemperature pH <7.
Exposure Check blood glucose By 24 hours- ketonaemia + acidosis should have HCO3 <
If blood glucose <3 mmol/L, give glucose IV and Ketone
resolved
recheck blood glucose Ix
Assess (tone), breathing, HR BM + k
E: Conversion to subcutaneous insulin metabo
Diagnosis (T wav
Acute onset of illness Vascular access No vascular
Airway swelling, hoarseness, stridor Lorazepram 0.1 mg/kg access If gasping/not breathing
Breathing tachypnoea, wheeze, cyanosis, Diazepam 0.5mg/kg Give 5 inhalation breaths
SpO2 <92% PR Consider SpO2 +/- ECG
OR midazolam
Circulation pale, clammy, hypotension, No response in 10
drowsy, coma mins
(buccal) 0.5 mg/kg
DK
Skin changes Re-assess
+/- GI symptoms If no increase in HR look for chest
Lorazepram 0.1mg/kg IV movement during inflation
No response in 10 mins
If chest not moving When the chest A:
Re-check head is moving
Call for help position
Res
Paraldehyde 0.4 ml/kg PR Consider 2-person
If the HR is not ove
airway control + detectable/is Mo
other airway very slow Pot
Lie patient flat and raise legs (if breathing manoeuvres (<60/min) Com
not impaired) No response in 10 mins Repeat inflation
Call for senior help ventilate for 30
breaths
SpO2 +/- ECG
seconds
Look for a response
Adrenaline (1:1000)
Phenytoin
Phenobarbital Reassess HR
Sodium valproate If still <60/min start chest
compressions; coordinate with
If available Monitor ventilation breaths (ratio 3:1)
Establish airway Pulse oximetry
High flow O2 ECG
Blood pressure Call anaesthetist/ no response in 20
IV fluid (20ml/kg mins
crystalloids) Re-assess HR every 30 seconds
Chlorpheniramine (IM/slow Rapid-sequence induction with thiopental If HR is not detectable/ very slow
IV) Mechanical ventilation (<60/min) consider venous
Hydrocortisone (IM/ slow Transfer to PICU access/drugs
IV)