Carlos Vendrell
Clinical Neuroscience – Best notes ever
1. Pills N’ Potions
Pharmacological treatment of brain disorders
Gribkoff et al 2017 Neuropharmacology
“The fact that drugs treat symptoms but do not affect the disease process would be fine if the
drugs had few if any side effects impacting quality of life or drug compliance, had no abuse
potential, did not often induce tachyphylaxis or other forms of drug resistance, and were not
economically challenging to individuals or healthcare systems.” However, most of the
pharmacological treatments of brain disorders are limited or temporary efficacy and with side-
effects. Main drawbacks observed on CNS drugs:
• Little to no effect on disease progression
• Almost all available treatments are symptomatic
• Chronic and continuous treatment is necessary
• Problem of heterogeneity, many patients are treatment-resistant
• Expensive (>1€billion) and long time needed for drug development (12-15 years)
In addition to the cons already mentioned another six reasons explain why CNS drugs
developments used to fail:
1) Lack of understanding of disease-mechanisms. Solution → target identification and
validation
2) Non-representative animal models
3) Blood Brain Barrier
4) Lack of biomarkers. Solution → stratification of populations for clinical trial
5) Subjectivity of end point measures
6) Regulatory restrictions
1) Drug design
Traditionally drugs were designed by trial-and-error testing of chemical substances in vitro, cell
cultures and animal models. Serendipity (random and fortune discovery) has played a crucial
role in the discovery of prototype psychotropic drugs that led to modern pharmacological
treatment in psychiatry (i.e. viagra, penicillin).
Nowadays (mid 90’s) drugs design has given way to a rational drug design, designing new drug
compounds based on the known properties of the biological ligand or target to achieve a
hypothesized therapeutic effect, also possible thanks to the advanced imaging techniques and
computer models. Thus, the serendipity factor is now much rarer due to the rise of rational drug
design but also because there is less time for clinicians to observe patients and the effects of
drugs and the reliance on double-blind placebo control randomized controlled trials. However,
still today the etiology for almost all brain disorders is unknown due to their complexity and
multifactorial cause (polygenic, environmental risks and interaction).
Because CNS drugs are relentless, ongoing degenerative disease processes, the established therapeutic
mechanisms depend on augmentation of some aspect of remaining circuitry to temporarily restore a
degree of function. When remaining circuits are sufficiently diminished, their efficacy disappears.
1
,Carlos Vendrell
2) Animal models
Animal models are useful and still necessary for pharmacodynamics, pharmacokinetics and
study of basic anatomy and physiology. However, there are extensive limitations on the
translation of animal model to human disease (good for studying molecular pathways and effect
of treatment studies but not for psychiatric behaviours). Therefore, industry has started to move
away from animal models (i.e. iPSCs, organoids)
3) Blood Brain Barrier
To develop an effective drug this one must overcome some impediments; it has to be small,
non-polar and lipophilic to cross the BBB and be delivered into the target area of the brain.
4) Biomarkers
Not all patients with the same diagnosis have the same disease or the same genetic/molecular
disturbance and therefore they can not be treated in the same way (heterogeneity).
Neurological diseases and psychiatric disorders show significant overlap in pathophysiology.
Biomarkers (i.e. molecules/proteins in blood or CSF, neuroimaging) are used to solve this
problem and differentiate between subpopulations or patients with different disease but similar
phenotype, allowing the selection of potential drug responders by identifying homogenous
subtypes.
5) End points measures
Neuropsychological testing, clinical evaluation and questionnaires show problems regarding to
test-retest effects, inter-rater variability and quite often are disconnected from real-life
functioning. Need for objective end point measures representative of function.
6) Rules and regulations
Complex and inconsistent regulations within and among agencies (e.g. FDA and EMA).
Negative pre-clinical findings are not published.
Non-pharmacological treatment of brain disorders
Non-pharmacological treatment is booming!! (i.e. Physical (dance) therapy, bright light therapy,
(cognitive) behavioural therapy, cognitive (strategy) training, neurostimulation, music therapy,
(multi) sensory stimulation, smart-home /assistive technology, acupuncture, nutrition).
Based on known pathophysiology mechanism. Often as adjuvant to pharmacological treatment
(generally improves efficacy)
Benefits: Less adverse effects, patients are part of their own treatments (increase efficacy),
cheaper, equally or more effective than drugs (many academic studies are currently being
conducted to test their efficacy).
Disadvantages: Generally, not disease-modifying, patients are part of their own treatment
(requires patient motivation, willing and healthy enough). NOT USEFUL FOR ALL DISEASES
Very few studies compare pharmacological/non-pharmacological treatments.
2
,Carlos Vendrell
COGTIPS – Cognitive training in Parkinson’s disease
BEWARE – Acceptance and commitment therapy in Parkinson’s disease
arrIBA – interference Based Approach therapy in OCD
TIPPICO – Transcranial magnetic stimulation + exposure therapy in OCD
PROSPER – CBT/EMDR in PTSD + personality disorders
EMDR (Eye Movement Desensitization and Reprocessing) + sleep therapy for PTSD
Bergen – intensive CBT (4 days) for OCD
Bright Light therapy for depression and sleep in Parkinson’s disease
MOTAR – running therapy for major depressive disorder (GGZ)
HIIT PD – High Intensity Interval Training for depression/cognition in PD
Bright Light therapy for depression and sleep in Parkinson’s disease
Light therapy is used to expose your eyes to intense but safe amounts of light for a specific
and regular length of time to “re-set” the circadian rhythm.
Treatment used for people who suffer from circadian rhythm sleep disorders. Your body has an
internal clock (“pacemaker”) at the suprachiasmatic nucleus that tells it when it is time to be
asleep and when it is time to be awake. These rhythms include body temperature, alertness and
the daily cycle of many hormones. Circadian disturbances in PD: Lower body temperature,
increased cortisol synthesis and flattened diurnal secretory curve, lower expression of clock
gene BMAL1 in PD, parkinsonian symptoms show circadian fluctuations (worse in
afternoon/evening), time-dependent response to antiparkinsonian medication.
Among other factors, your clock is “set” by your exposure to bright light such as sunlight
(captured by the retino-hypothalamic tract, RHT). Exposure to bright light or “light therapy” is
one method used to treat people with a circadian rhythm sleep disorder. Light therapy can help
someone “re-set” a clock that is off.
3
, Carlos Vendrell
Example of a randomized controlled trial in PD:
83 diagnosed PD patients
meeting the DSM-IV criteria
for MDD.
Randomized Controlled Trial
Comparison of two different
light conditions
3 months home treatment
30 minutes morning &
evening light
6 months follow-up
No differences between bright light therapy and placebo at the end of the experiment. Bright
light stimuli don’t work directly as therapy for depression. However, during these experiments
the circadian system of patients changed (woke up earlier and went to bed earlier). Routine and
wake up early is better for depression?
Conclusions
Disturbance of circadian rhythm contributes to
depression and sleeping problems in PD
MDD (severity) improved after both interventions
(due to day structuring?)
Light therapy improved subjective sleep quality,
presumably by reducing total cortisol secretion.
4
Clinical Neuroscience – Best notes ever
1. Pills N’ Potions
Pharmacological treatment of brain disorders
Gribkoff et al 2017 Neuropharmacology
“The fact that drugs treat symptoms but do not affect the disease process would be fine if the
drugs had few if any side effects impacting quality of life or drug compliance, had no abuse
potential, did not often induce tachyphylaxis or other forms of drug resistance, and were not
economically challenging to individuals or healthcare systems.” However, most of the
pharmacological treatments of brain disorders are limited or temporary efficacy and with side-
effects. Main drawbacks observed on CNS drugs:
• Little to no effect on disease progression
• Almost all available treatments are symptomatic
• Chronic and continuous treatment is necessary
• Problem of heterogeneity, many patients are treatment-resistant
• Expensive (>1€billion) and long time needed for drug development (12-15 years)
In addition to the cons already mentioned another six reasons explain why CNS drugs
developments used to fail:
1) Lack of understanding of disease-mechanisms. Solution → target identification and
validation
2) Non-representative animal models
3) Blood Brain Barrier
4) Lack of biomarkers. Solution → stratification of populations for clinical trial
5) Subjectivity of end point measures
6) Regulatory restrictions
1) Drug design
Traditionally drugs were designed by trial-and-error testing of chemical substances in vitro, cell
cultures and animal models. Serendipity (random and fortune discovery) has played a crucial
role in the discovery of prototype psychotropic drugs that led to modern pharmacological
treatment in psychiatry (i.e. viagra, penicillin).
Nowadays (mid 90’s) drugs design has given way to a rational drug design, designing new drug
compounds based on the known properties of the biological ligand or target to achieve a
hypothesized therapeutic effect, also possible thanks to the advanced imaging techniques and
computer models. Thus, the serendipity factor is now much rarer due to the rise of rational drug
design but also because there is less time for clinicians to observe patients and the effects of
drugs and the reliance on double-blind placebo control randomized controlled trials. However,
still today the etiology for almost all brain disorders is unknown due to their complexity and
multifactorial cause (polygenic, environmental risks and interaction).
Because CNS drugs are relentless, ongoing degenerative disease processes, the established therapeutic
mechanisms depend on augmentation of some aspect of remaining circuitry to temporarily restore a
degree of function. When remaining circuits are sufficiently diminished, their efficacy disappears.
1
,Carlos Vendrell
2) Animal models
Animal models are useful and still necessary for pharmacodynamics, pharmacokinetics and
study of basic anatomy and physiology. However, there are extensive limitations on the
translation of animal model to human disease (good for studying molecular pathways and effect
of treatment studies but not for psychiatric behaviours). Therefore, industry has started to move
away from animal models (i.e. iPSCs, organoids)
3) Blood Brain Barrier
To develop an effective drug this one must overcome some impediments; it has to be small,
non-polar and lipophilic to cross the BBB and be delivered into the target area of the brain.
4) Biomarkers
Not all patients with the same diagnosis have the same disease or the same genetic/molecular
disturbance and therefore they can not be treated in the same way (heterogeneity).
Neurological diseases and psychiatric disorders show significant overlap in pathophysiology.
Biomarkers (i.e. molecules/proteins in blood or CSF, neuroimaging) are used to solve this
problem and differentiate between subpopulations or patients with different disease but similar
phenotype, allowing the selection of potential drug responders by identifying homogenous
subtypes.
5) End points measures
Neuropsychological testing, clinical evaluation and questionnaires show problems regarding to
test-retest effects, inter-rater variability and quite often are disconnected from real-life
functioning. Need for objective end point measures representative of function.
6) Rules and regulations
Complex and inconsistent regulations within and among agencies (e.g. FDA and EMA).
Negative pre-clinical findings are not published.
Non-pharmacological treatment of brain disorders
Non-pharmacological treatment is booming!! (i.e. Physical (dance) therapy, bright light therapy,
(cognitive) behavioural therapy, cognitive (strategy) training, neurostimulation, music therapy,
(multi) sensory stimulation, smart-home /assistive technology, acupuncture, nutrition).
Based on known pathophysiology mechanism. Often as adjuvant to pharmacological treatment
(generally improves efficacy)
Benefits: Less adverse effects, patients are part of their own treatments (increase efficacy),
cheaper, equally or more effective than drugs (many academic studies are currently being
conducted to test their efficacy).
Disadvantages: Generally, not disease-modifying, patients are part of their own treatment
(requires patient motivation, willing and healthy enough). NOT USEFUL FOR ALL DISEASES
Very few studies compare pharmacological/non-pharmacological treatments.
2
,Carlos Vendrell
COGTIPS – Cognitive training in Parkinson’s disease
BEWARE – Acceptance and commitment therapy in Parkinson’s disease
arrIBA – interference Based Approach therapy in OCD
TIPPICO – Transcranial magnetic stimulation + exposure therapy in OCD
PROSPER – CBT/EMDR in PTSD + personality disorders
EMDR (Eye Movement Desensitization and Reprocessing) + sleep therapy for PTSD
Bergen – intensive CBT (4 days) for OCD
Bright Light therapy for depression and sleep in Parkinson’s disease
MOTAR – running therapy for major depressive disorder (GGZ)
HIIT PD – High Intensity Interval Training for depression/cognition in PD
Bright Light therapy for depression and sleep in Parkinson’s disease
Light therapy is used to expose your eyes to intense but safe amounts of light for a specific
and regular length of time to “re-set” the circadian rhythm.
Treatment used for people who suffer from circadian rhythm sleep disorders. Your body has an
internal clock (“pacemaker”) at the suprachiasmatic nucleus that tells it when it is time to be
asleep and when it is time to be awake. These rhythms include body temperature, alertness and
the daily cycle of many hormones. Circadian disturbances in PD: Lower body temperature,
increased cortisol synthesis and flattened diurnal secretory curve, lower expression of clock
gene BMAL1 in PD, parkinsonian symptoms show circadian fluctuations (worse in
afternoon/evening), time-dependent response to antiparkinsonian medication.
Among other factors, your clock is “set” by your exposure to bright light such as sunlight
(captured by the retino-hypothalamic tract, RHT). Exposure to bright light or “light therapy” is
one method used to treat people with a circadian rhythm sleep disorder. Light therapy can help
someone “re-set” a clock that is off.
3
, Carlos Vendrell
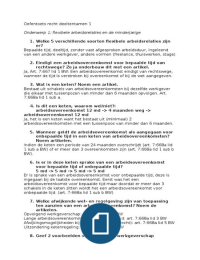
Example of a randomized controlled trial in PD:
83 diagnosed PD patients
meeting the DSM-IV criteria
for MDD.
Randomized Controlled Trial
Comparison of two different
light conditions
3 months home treatment
30 minutes morning &
evening light
6 months follow-up
No differences between bright light therapy and placebo at the end of the experiment. Bright
light stimuli don’t work directly as therapy for depression. However, during these experiments
the circadian system of patients changed (woke up earlier and went to bed earlier). Routine and
wake up early is better for depression?
Conclusions
Disturbance of circadian rhythm contributes to
depression and sleeping problems in PD
MDD (severity) improved after both interventions
(due to day structuring?)
Light therapy improved subjective sleep quality,
presumably by reducing total cortisol secretion.
4