A patient enters the emergency department in respiratory compromise. The team is
monitoring the patient using capnography and identifies that ETCO2 levels are initially 33
mmHg and later 40 mmHg. From these readings, the team identifies that the patient is
progressing in what stage of respiratory compromise?
Respiratory arrest
Respiratory failure
Respiratory distress
Respiratory acidosis
Respiratory distress
Capnography can objectively assess the severity of a patient's respiratory
distress. Early on, the patient will often hyperventilate, leading to hypocapnia
that is reflected by a low ETCO2 value (less than 35 mmHg). As respiratory
distress increases, and the patient begins to tire, the ETCO2 value may return
to the normal range (35 to 45 mmHg). However, if the patient progresses to
, respiratory failure, the ETCO2 level will increase to greater than 45 mmHg,
which indicates hypoventilation.
A responsive patient is choking. What method should the provider use first to clear the
obstructed airway?
Back blows
Abdominal thrusts
Magill forceps extraction
Chest compressions
Back blows
To clear an obstructed airway in a responsive adult, first provide up to 5 back
blows to clear the obstruction.
A patient is receiving ventilation support via bag-valve-mask (BVM) resuscitator.
Capnography is established and a blood gas is obtained to evaluate the adequacy of the
ventilations. Which arterial carbon dioxide (PaCO2) value signifies adequate ventilations?
10 to 15 mmHg
20 to 25 mmHg
25 to 30 mmHg
35 to 45 mmHg
, 35 to 45 mmHg
Arterial carbon dioxide (PaCO2) values in the range of 35 to 45 mmHg
confirm adequacy of ventilation.
A 42-year-old woman presents to the emergency department with complaints of fatigue,
shortness of breath, back pain and nausea. A 12-lead ECG is obtained and shows ST-
segment depression in leads II, III, and aVF and intermittent runs of nonsustained
ventricular tachycardia. Cardiac serum markers are elevated. These findings suggest
which condition?
High-risk non-ST-segment elevation ACS (NSTE-ACS)
Low-risk non-ST-segment elevation ACS (NSTE-ACS)
Intermittent-risk non-ST-segment elevation ACS (NSTE-ACS)
ST-segment elevation myocardial infarction (STEMI)
High-risk non-ST-segment elevation ACS (NSTE-ACS)
The 12-lead ECG findings of ST-segment depression in three contiguous leads
along with elevated cardiac serum biomarkers are consistent with high-risk
non-ST-segment elevation ACS (NSTE-ACS). The presence of intermittent runs
of ventricular tachycardia also places this patient at high risk. In ST-segment
elevation myocardial infarction (STEMI), cardiac serum markers would be
elevated, but this patient's ECG findings are not consistent with STEMI. Patients
with intermediate- or low-risk NSTE-ACS show nondiagnostic ST-segment or
T-wave changes on ECG, or no changes at all.
The stroke team is assessing a patient with a suspected stroke. The patient is alert and
able to carry on a conversation, although the patient has difficulty getting the words out.
, Testing confirms that the patient has had an ischemic stroke. Based on the patient's
medical history, a history of which arrhythmia would alert the team to the patient's
increased risk for stroke?
Atrial fibrillation
Atrial tachycardia
Ventricular fibrillation
Bradycardia
Atrial fibrillation
Between 15 and 20 percent of embolic strokes are caused by atrial fibrillation.
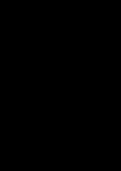
A patient in the telemetry unit is receiving continuous cardiac monitoring. The patient has
a history of myocardial infarction. The patient's ECG rhythm strip is shown in the
following figure. The provider interprets this strip as indicating which arrhythmia?
Sinus tachycardia
Third-degree AV block
First-degree atrioventricular (AV) block
Second-degree AV block
Third-degree AV block
In third-degree AV block, no electrical communication occurs between the
atria and ventricles, thus no relationship between P waves and QRS complexes
exists. The RR interval is constant. The PP interval is constant or slightly
irregular, as with sinus arrhythmia. If pacemaker cells in the AV junction
simulate ventricular contraction, the QRS complexes will be narrow (less than
120 milliseconds in duration). Impulses that originate in the ventricles produce