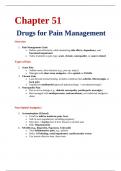
Drugs for Pain Management
Overview
1. Pain Management Goals
o Relieve pain effectively while minimizing side effects, dependency, and
functional impairment
o Tailor treatment to pain type: acute, chronic, neuropathic, or cancer-related
Types of Pain
2. Acute Pain
o Sudden onset, short duration (e.g., post-op, injury)
o Managed with short-term analgesics, often opioids or NSAIDs
3. Chronic Pain
o Lasts beyond normal healing; includes conditions like arthritis, fibromyalgia, or
back pain
o Emphasizes multimodal approach (pharmacologic + non-pharmacologic)
4. Neuropathic Pain
o Due to nerve damage (e.g., diabetic neuropathy, postherpetic neuralgia)
o Best managed with antidepressants, anticonvulsants, not traditional analgesics
alone
Non-Opioid Analgesics
5. Acetaminophen (Tylenol)
o Good for mild to moderate pain, fever
o Safe in most populations, including pregnancy
o Max dose: <4 g/day (less if liver disease or alcohol use)
o Risk: Hepatotoxicity
6. NSAIDs (e.g., Ibuprofen, Naproxen, Celecoxib)
o Treat inflammatory pain, e.g., arthritis
o Risks: GI bleeding, renal impairment, cardiovascular events
o Use lowest effective dose, short-term
,Opioid Analgesics
7. Examples: Morphine, Oxycodone, Hydrocodone, Fentanyl
o Used for moderate to severe pain
o Act on mu-opioid receptors in CNS
o Monitor for sedation, respiratory depression, constipation
8. Adverse Effects
o Nausea, itching, urinary retention, tolerance, dependence
o Use bowel regimen for constipation (e.g., stool softeners, laxatives)
9. Opioid Risk Management
o Evaluate risk of abuse or misuse
o Consider prescription monitoring programs (PMPs)
o Taper gradually to avoid withdrawal
Opioid Antagonists
10. Naloxone (Narcan)
Reverses opioid overdose rapidly
Available as nasal spray, IM, or IV
Short half-life—may need repeat doses
Adjuvant Medications
11. Antidepressants
Amitriptyline, Duloxetine help with neuropathic and chronic pain
Work by increasing serotonin/norepinephrine in CNS
Side effects: Dry mouth, sedation, dizziness
12. Anticonvulsants
Gabapentin, Pregabalin
Reduce nerve excitability
Often used in diabetic neuropathy, fibromyalgia, shingles pain
Side effects: Sedation, weight gain
13. Topical Agents
Lidocaine patches, Capsaicin cream
Useful in localized pain; fewer systemic effects
, 14. Muscle Relaxants
Cyclobenzaprine, Tizanidine
For spasticity or muscle-related pain
Can cause drowsiness, dry mouth, hypotension
Chronic Pain Management Strategies
15. Multimodal Approach
Combine meds, physical therapy, psychological support
Avoid sole reliance on opioids
16. Opioid Use in Chronic Pain
Use lowest effective dose
Regularly reassess function and risks
Consider opioid agreements and urine drug screens
Pain Management in Special Populations
17. Older Adults
More sensitive to side effects
Prefer acetaminophen, topicals, and low-dose opioids if needed
18. Pregnancy
Acetaminophen is safest
Avoid NSAIDs in third trimester
Opioids used only when benefits outweigh risks
19. Patients with History of Substance Use
Use non-opioid strategies whenever possible
Consider involving addiction specialists
Patient Education
20. Proper Use of Pain Meds
, Take as prescribed; don’t crush long-acting opioids
Avoid alcohol or sedatives when on opioids
21. Non-Drug Approaches
Encourage exercise, CBT, heat/cold, mindfulness
22. Monitoring and Follow-Up
Reevaluate pain level, function, and adverse effects regularly
Adjust treatment plan based on patient response